Photo credit @profwicks
WHAT YOU NEED TO KNOW ABOUT ADHD
Statistics: Did You Know? (Child &/ Adolescent)
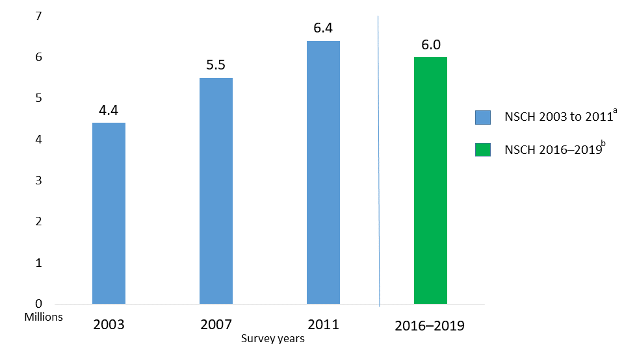
Millions of US children have been diagnosed with ADHD.
The estimated number of children aged 3–17 years ever diagnosed with ADHD, according to a national survey of parents,1 is 6 million (9.8%) using data from 2016-2019. This number includes:
3–5 years: 265,000 (2%)
6–11 years 2.4 million (10%)
12–17 years: 3.3 million (13%).
Boys (13%) are more likely to be diagnosed with ADHD than girls (6%).1
Black, non-Hispanic children and White, non-Hispanic children are more often diagnosed with ADHD (12% and 10%, respectively), than Hispanic children (8%) or Asian, non-Hispanic children (3%).1
Estimated number of U.S. children ages 3–17 years who ever had a diagnosis of ADHD,1 in millions.
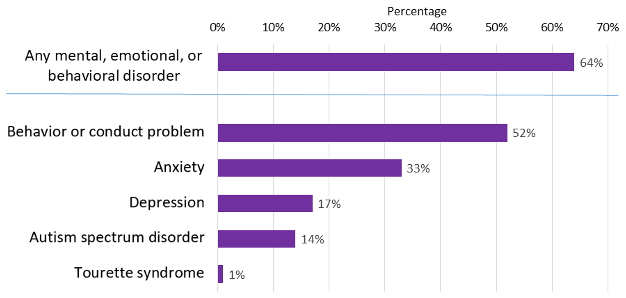
According to a national 2016 parent survey,1 6 in 10 children with ADHD had at least one other mental, emotional, or behavioral disorder:
About half of the children with ADHD had a behavior or conduct problem.
About 3 in 10 children with ADHD had anxiety.
Percent of children with ADHD who had at least one other disorder. (2)
Statistics: Did You Know?
· Teen drivers diagnosed with ADHD are more likely to be in a traffic accident, be issued traffic and moving violations, and engage in risky driving behaviors.3
· Up to 27 percent of adolescents with substance abuse disorder have comorbid ADHD.4
· Adolescents with ADHD clash with their parents about more issues than do adolescents without ADHD.5
· Adolescent girls with ADHD are more likely to struggle with social difficulties and have a poor self-concept compared to boys with ADHD and women without ADHD.6
· Teen boys with ADHD are more likely to experience problems with attendance, GPA, homework, and more in high school.7
o Male teens with ADHD miss school 3 to 10 percent of the time;
o Are between 2.7 and 8.1 times more likely to drop out of high school;
o More likely to fail 7.5 percent of their courses;
o Usually have GPAs five to nine points lower than those of male teens without ADHD.
· Approximately 2 to 8 percent of college students self-report clinically significant symptoms associated with ADHD.8
Symptomology: What is ADHD? (Child &/ Adolescent)
ADHD or attention deficit hyperactivity disorder is a very common neurodevelopmental (brain development) disorder of childhood. It is usually first diagnosed in childhood and often lasts into adulthood. But many individuals are diagnosed as adults because some parents may look at the behaviors as simply disobedience instead of a mental health condition. Children with ADHD may have trouble paying attention or focusing, staying organized, controlling impulsive behaviors (act first, think later), or be overly active (hyper) in comparison to their peers.
Some symptoms of ADHD can be normal child behavior so it’s important to note these behaviors occur more often than their peers.
Often daydream
Often forget or lose things
Often squirm or fidget
Often talk too much
Often make careless mistakes or take unnecessary risks
Often have a hard time resisting temptation
Often have trouble waiting their turn
Often have difficulty getting along with others
Outlook: Untreated and Undiagnosed ADHD in Children (Child &/ Adolescent)
ADHD is not something children grow out of. If left untreated ADHD can lead to childhood behavioral disorder known as oppositional defiant disorder (ODD). Statistics show 40 percent of children with ADHD also develop ODD.
“Many kids with ADHD who are diagnosed with ODD are showing oppositional characteristics by default,” says Houston-based child psychologist Carol Brady, Ph.D. “They misbehave not because they’re intentionally oppositional, but because they can’t control their impulses.”
Other experts suggest that ODD is a way for kids to cope with the frustration and emotional pain associated with having ADHD due to feelings of low self-esteem and perceived rejection.
In children with Oppositional Defiant Disorder (ODD), there is an ongoing pattern of uncooperative, defiant, and hostile behavior toward authority figures that seriously interferes with the child's day to day functioning.
Symptoms of ODD may include:
Frequent temper tantrums
Excessive arguing with adults
Often questioning rules
Active defiance and refusal to comply with adult requests and rules
Deliberate attempts to annoy or upset people
Blaming others for his or her mistakes or misbehavior
Often being touchy or easily annoyed by others
Frequent anger and resentment
Mean and hateful talking when upset
Spiteful attitude and revenge seeking
The symptoms are usually seen in multiple settings but may be more noticeable at home or at school. One to sixteen percent of all school-age children and adolescents have ODD.
Interventions: How we can Help (Child &/ Adolescent)
Parent Management Training to help parents and others manage their child's behavior
Individual Psychotherapy to develop more effective symptom management
Family Psychoeducation to improve communication and mutual understanding
Cognitive Problem-Solving Skills to decrease negative outcomes
Social Skills Training to increase flexibility and improve social skills and frustration tolerance with others.
We can discuss alternatives to medications that you can try while also acknowledging that medications may be helpful in controlling some of the more distressing symptoms of ADHD as well as the symptoms related to coexistent conditions such as ODD, anxiety, and mood disorders and we recommend speaking with your medical doctor regarding any regimen of supplements or medication.
References
1. Bitsko RH, Claussen AH, Lichstein J, et al. Mental health surveillance among children—United States, 2013–2019. MMWR Suppl. 2022;71(2):1-48.
2. Visser, SN Danielson ML, Wolraich ML, Fox M, Grosse SD, Valle LA, Holbrook JR, Claussen AH, Peacock, P. Vital signs: National and state-specific patterns of attention deficit/hyperactivity disorder treatment among insured children aged 2–5 years — United States, 2008–2014. Morbidity and Mortality Weekly Report (MMWR); 2016,65, 443–450.
3. Curry, A., Yerys, B., Metzger, K., et. al. (June 2019). Traffic Crashes, Violations, and Suspensions Among Young Drivers With ADHD. Pediatrics. 143 (6) e20182305; DOI: 10.1542/peds.2018-2305. Retrieved from: https://pediatrics.aappublications.org/content/143/6/e20182305
4. van Emmerik-van Oortmerssen, K., van de Glind, G., van den Brink, W., Smit, F., Crunelle, C. L., Swets, M., Schoevers, R. A. (April 2012). Prevalence of Attention-Deficit Hyperactivity Disorder in Substance Use Disorder Patients: A Meta-Analysis and Meta-Regression Analysis. Drug and Alcohol Dependence. Volume 122, Issues 1–2. Pages 11-19. doi:10.1016/j.drugalcdep.2011.12.007. Retrieved from: https://www.sciencedirect.com/science/article/abs/pii/S0376871611005291?via%3Dihub
5. Markel, C., Wiener, J. (2014). Attribution Processes in Parent-Adolescent Conflict in Families of Adolescents With and Without ADHD. Canadian Journal of Behavioural Science/Revue Canadienne Des Sciences Du Comportement. 46, 40-48. doi:10.1037/a0029854. Retrieved from: https://psycnet.apa.org/record/2012-30261-001?doi=1
6. Holthe, M. E. G., & Langvik, E. (2017). The Strives, Struggles, and Successes of Women Diagnosed With ADHD as Adults. SAGE Open. https://doi.org/10.1177/2158244017701799
7. Kent, Kristine M et al. (April 2011). The Academic Experience of Male High School Students with ADHD. Journal of Abnormal Child Psychology. Volume 39, 3. 451-62. doi:10.1007/s10802-010-9472-4. Retrieved from: https://link.springer.com/article/10.1007/s10802-010-9472-4
8. DuPaul, G. J., Weyandt, L. L., O’Dell, S. M., & Varejao, M. (2009). College Students With ADHD: Current Status and Future Directions. Journal of Attention Disorders. 13(3), 234–250. https://doi.org/10.1177/1087054709340650. Retrieved from: https://journals.sagepub.com/doi/abs/10.1177/1087054709340650